Abstract
Introduction: MF is a Philadelphia-negative myeloproliferative neoplasm (Ph-negative MPN) with an heterogeneous outcome. In 2009, Cervantes et al. published the International Prognostic Score System (IPSS) to better determine outcomes in this disease. In the last decade, several recurrently mutated genes have been described in MF, some of them associated with prognostic impact in survival. We propose a novel prognostic score that incorporates molecular and cytogenetic data in patients with MF.
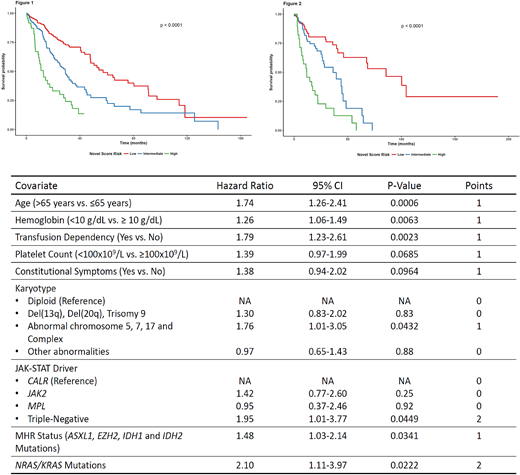
Methods: We analyzed clinical, cytogenetic and molecular data from 623 patients with a diagnosis of primary MF (N=445), post-PV MF (N=109) and post-ET MF (N=69). Data was extracted from medical records at time of sample collection for analysis. Mutation data was obtained by next-generation sequencing analysis, performed with either paired tumor-normal whole exome sequencing (N=46) or selected gene panel for genes associated with myeloid malignancies (N=577). The following 16 genes were analyzed in all 623 patients and were considered as the common denominator for analysis: ASXL1, CALR, DNMT3A, EZH2, FLT3, IDH1, IDH2, JAK2, KIT, KRAS, MPL, NRAS, RUNX1, TET2, TP53, WT1. RAS mutations were considered as oncogenic mutations in NRAS and/or KRAS. Molecular high risk (MHR) mutations were considered as mutations in any one of the 4 genes: ASXL1, EZH2, IDH1, IDH2 (SRSF2 mutations were not included since they were not evaluated in all cases). Cytogenetic data was stratified into 4 risk categories (based on Tam et al, Blood 2009): (1) Diploid; (2) Del(13q)/Del(20q)/Trisomy 9; (3) Abnormalities of chromosomes 5, 7, 17 and complex karyotype; (4) Other abnormalities. To develop the model, the data was split into a training dataset (N=434) and a test dataset (N=189). Variables initially included in the initial training model were those with a p-value<0.05 in the univariate analysis; subsequently, this initial model was internally validated with a bootstrap procedure for stepwise backwards selection and determination of variables to be included the final model. Score points were assigned based on the value of the hazard ratio (HR). The final model was externally validated in the test dataset. Akaike information criterion (AIC) was calculated on the final model and on the Dynamic IPSS (DIPSS) model on the full dataset, and the best model was considered the one with the lowest AIC value and the highest AIC weight.
Results: In the training cohort, after a median follow-up of 30.8 months, there were 176 deaths (40.5%). The initial variables included in the multivariate Cox model were: age (>65 years), hemoglobin (<10 g/dL), white blood cell count (WBC; >25x109/L), peripheral blood blasts (>1%), presence of constitutional symptoms, sex (male vs female), platelet count (<100x109/L), type of JAK-STAT driver mutation (CALR vs JAK2 vs MPL vs Triple-negative), karyotype risk category, presence of MHR mutations and presence of RAS mutations. After bootstrapping, variables sex, peripheral blood blasts and WBC were excluded, and the final model with associated HRs is presented on table 1. Since most HRs were near 1, 1-point was given to each variable, with the exception of Triple-negative molecular status and RAS mutations (2 points each). We grouped patients based on similarity of HR into three risk categories: low (0-2 points; N=243), intermediate (3-4 points, N=141) and high (5+ points, N=50). These 3 groups were associated with significantly different survival outcomes (Figure 1): 3-years OS was 71% (95% CI 64-78%), 38% (95% CI 29-50%) and 18% (95% CI 9-37%) for low, intermediate and high risk groups (P=1.33e-13). Validating the model on the test dataset revealed significantly differences in OS among the 3 risk categories (Figure 2): 74% (95% CI 63-86%), 50% (95% CI 36-68%) and 16% (95% CI 6-39%) (P=1.42e-11). Analyzing the full dataset, the novel score model had a lower AIC than the DIPSS model (2713 vs 2722) and a higher AIC weight (0.99 vs. 0.01).
Conclusion: Incorporating molecular data, including MHR mutations, karyotype and RAS mutations leads to the development of an improved prognostic model. Further validation of this model in other cohorts is necessary. The impact of novel therapies should be evaluated among the different risk categories.
Rampal:Stemline: Research Funding; Celgene: Honoraria; Constellation: Research Funding; Incyte: Honoraria, Research Funding; Jazz: Consultancy, Honoraria. Verstovsek:Celgene: Membership on an entity's Board of Directors or advisory committees; Italfarmaco: Membership on an entity's Board of Directors or advisory committees; Novartis: Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Incyte: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal